Integrative Multimodal Treatment
Concepts For Polyneuropathy
From Three Specialized Institutions
Summary
In relation to conventional pain therapy, the concepts presented by the three renowned institutions show new and comprehensive ways of treating and coping with polyneuropathy, which is often very restrictive and painfully experienced.
These facilities place the person at the center of therapy – not just the affected extremity(s) – and motivate and enable them to their highest possible self-control.
Some therapeutic methods have been used in all three clinics for a long time, which should encourage imitation. All other approaches presented could be supplemented according to individual knowledge and treatment context.
There is no one right way to deal with this common disease with sometimes severe pain. The person is too individual for that, and the diagnosis, the cause of the disease, the clinical picture and the pain processing of polyneuropathy are far too diverse.
In the case of polyneuropathies, every building block for alleviation counts – complementary medicine multimodal approaches show new treatment possibilities.
Introduction
The overall prevalence of patients with polyneuropathy (PNP) is estimated to be 4% in the general population, rising to up to 13% in people aged 80 and over. The number of patients with polyneuropathy is expected to increase due to the aging population and increasing prevalence rates of known risk factors for polyneuropathy such as diabetes, adiposity (obesity), and cardiovascular disease [1].
Polyneuropathy is a generalized disease of the peripheral nerves that can lead to motor, sensory and vegetative deficits. The causes can be manifold. These include metabolic diseases, malnutrition, inflammatory and tumorous diseases, toxic substances, medications and hereditary diseases. Idiopathic polyneuropathy, in which no underlying cause can be found, is particularly common in old age. Exact figures specifically for this form are difficult to determine, as polyneuropathy is very common overall and the diagnosis of causes varies [2].
The diagnosis of neuropathic pain is based on the typical symptoms and findings of neuropathic pain, in particular the combination of deficit symptoms (sensory deficits such as hypoesthesia, hypoalgesia) and positive symptoms (burning pain, especially at rest, shooting pain attacks, allodynia, hyperalgesia).
Depending on the medical history and clinical findings, specific diagnostics can be carried out. However, a causal therapy that usually leads to freedom from symptoms is rather rare, also in view of the often already existing nerve damage (axonal, demyelicating).
Thus, symptom relief is often at the forefront of therapeutic efforts. The often excruciating pain is treated with analgesics and the anticonvulsants and/or antidepressants often used for neuropathic pain. Other therapy goals include improvements in general lifestyle and measures that promote nerve blood flow, such as quitting smoking, regular exercise, reducing cardiovascular restrictions and improving nutrition. However, it must be admitted that symptom relief is often difficult to achieve or lacks because most treatments only have a “medium” effect size [3].
Symptom relief for PNP is often difficult to achieve, conventional treatments only have a “medium” effect size.
This situation is made much more difficult if the neuropathic pain in PNP has become chronic. The sensitization of the peripheral and central nociceptive system and the existence of relevant psychosocial influencing factors make chronic pain a disease in its own right, which has been proven not to be adequately addressed by monomodal or purely drug measures.
Interestingly, the necessary multimodal concepts are found more in the field of integrative medicine in the sense of a rational synthesis of conventional and complementary procedures than in the field of the corresponding disciplines.
Three specialized institutions in Germany have particular experience in this area, which have been offering intensified, interdisciplinary and multimodal concepts for decades:
- the Hospital for Naturopathy (KfN), Munich-Harlaching **
- Immanuel Hospital Berlin, Berlin-Wannsee
- the Interdisciplinary Pain Outpatient Clinic and Day Clinic of the LMU Munich, Campus Innenstadt
All three facilities proceed according to a holistic understanding of illness and attach importance to the active cooperation of the patient in coping with the disease. Naturopathic and complementary procedures have proven themselves in these facilities for decades in order to ultimately alleviate suffering and improve the quality of life of those affected.
Treatment of Polyneuropathies At The Hospital for Naturopathy (KfN), Munich-Harlaching
An inpatient stay of an average of 10 treatment days at the KfN should lead to a significant improvement in general condition and symptoms of illness in the short term as well as enable sustainable treatment success for our patients, who are usually chronically ill. This also requires the implementation of long-term health-relevant lifestyle modifications and naturopathic self-help strategies. The basis of our so-called naturopathic complex treatment, which is covered by all health insurance companies, is “Lifestyle Regulation Therapy” (teaching of a healthy lifestyle), nutrition, exercise, relaxation and the learning of naturopathic self-help strategies. Since chronically ill patients can be admitted again and again, e.g. once a year, we can thus offer long-term complementary naturopathic support, of course not as a replacement, but as a sensible supplement to conventional therapies and in consultation with the treating general practitioners and/or specialists.
Our patient clientele also includes patients with PNP of different origins with painful paresthesia as the leading symptom. As a rule, these patients are neurologically clarified and more or less “exhausted”. They hope that a stay at the KfN will lead to new approaches to symptom relief and, ideally, disease control. In our experience, sustainable symptom relief of about 30-50% is an ambitious, but quite achievable goal.
The above-mentioned basic therapy modules are specifically supplemented by more specific naturopathic interventions in order to locally influence the damaged nociceptive c-fibers, which are decisive for the development of pain in PNP, and to reduce the central pain sensitization, which is additively responsible for chronification. Neuroregenerative processes should be stimulated by increasing the local microcirculation and the perception of neuropathic paresthesia is modulated by mechanical stimulation of tactile receptors (Gate Control Theory).
 Fig. 2 Lower leg shower in polyneuropathy. Source: D. Irnich
Fig. 2 Lower leg shower in polyneuropathy. Source: D. Irnich
These include, for example, hydrotherapy with cold or alternating warm showers, ascending partial baths or full baths with additives that promote blood circulation and thus support nerve function (among others spruce needles, hay flowers, Sulphur). Electrotherapy in the form of transcutaneous electrical nerve stimulation (TENS) as well as 2- and 4-cell baths aims to modulate pain conduction and promote nerve regeneration. CO2 baths are used for peripheral stimulation of the tissue, which leads to improved skin circulation and mild circulation stimulation. Probative moderate whole-body hyperthermia (mGKHT) can also be performed to relieve pain, but PNP is not one of the classic indications for mGKHT in our country [Germany].
Classical physiotherapy is another important part of PNP treatment. Through mobilization and targeted muscle building, muscular weaknesses and instability can be compensated. Sensorimotor-functional individual treatments can have a positive effect on surface and depth sensitivity, which in turn improves pain processing and reduces pain triggers. Occupational therapy measures, such as fine motor skills training, also support everyday coping. Foot reflexology massage can help improve symptoms in PNP via local mechanical stimuli and psychoneuroimmunological effects.
Nursing measures complement the therapy with local applications. Sugar oil or aromatic oil rubs (1-4 times a day) can help relieve pain. This is where their anti-inflammatory, antinociceptive and circulation-promoting properties come into play, e.g. of lavender, peppermint or eucalyptus oil. Pleasant scents and touch can also promote the release of endorphins, serotonin and oxytocin, which further reduces the sensation of pain and promotes relaxation. These oils are used in aqueous-alcoholic solutions for poultices, embrocations or as ointment preparations. (Heat) Red oil pads (St. John’s wort) traditionally have a strong connection to nervous disorders and have a comparable effect. Probative lavender or rosemary foot baths as well as clay packs and healing clay pads can also be used to relieve symptoms.
Cayenne pepper fruit (capsaicin) is used in ointments and heat patches and is approved in the EU for the treatment of peripheral neuropathic pain in patients who do not have diabetes mellitus. Capsaicin has a local hyperemic, analgesic, anti-inflammatory, cortisone-like and antipruritic effect. Through an almost complete release of substance P and subsequent inhibition of the transport and new synthesis of substance P, the conduction of pain is interrupted in the sense of desensitization of the nociceptors. Long-term low-dose or short-term high-dose therapy with capsaicin leads to histologically detectable retraction of the nociceptors, which explains the long-term pain-relieving effect. For dosages above 0.075% as well as for plasters and occlusive dressings, the duration of use should be limited to a maximum of 2 days, because irreversible damage to sensitive nerves can occur. For ointments or creams with a capsaicin content below 0.075%, it is recommended to apply them thinly to the skin 2-3 times a day. Patients should be advised of a marked initial burning of the skin and dysesthesia as possible side effects.
From an orthomolecular medicine point of view, PNP is characterized by a complex pathogenesis driven by axonal transport disorder, mitochondrial dysfunction, oxidative stress and the accumulation of so-called advanced glycation end products (AGEs). The application of specific micronutrients in therapeutic doses aims to optimize essential cellular processes and neutralize neurotoxic stress factors.
Alpha-lipoic acid (ALA) is a powerful antioxidant. It acts as a free radical scavenger of reactive oxygen and nitrogen species, thus helping to maintain glutathione redox status. It can also improve endoneural microcirculation, which counteracts the ischemic and hypoxic components of neuropathy. The clinical efficacy has been investigated in particular for intravenous administration in the therapy of diabetic polyneuropathy and has been anchored in the guideline for this indication for over 20 years. At KfN, we usually apply ALA 600 mg intravenously once a day for 5 days and then recommend oral administration of the same dose for at least 3 months followed by reevaluation.
With regard to neurotropic B vitamins (especially B1, B3, B6, B9, B12), levels in the upper normal range or slightly above are sought. Some recent research suggests that Vitamin B12 in particular promotes neuronal regeneration; The vitamin B complex is being investigated as a protective agent in chemotherapy-induced peripheral neuropathy.
Antioxidants such as Vitamins C and E can help reduce lipid peroxidation. We infuse Vitamin C several times in high doses (7.5 g) during the inpatient stay. Selenium is recommended as a cofactor of antioxidant enzymes and due to its potential neuroregenerative properties, which are also attributed to anti-inflammatory Omega-3 fatty acids.
Polyneuropathy patients should be motivated to take care of themselves in a sustainable way through information and training.
Ultimately, we try to develop a feasible, everyday treatment concept for the time after discharge together with the patient during the inpatient stay, taking into account the individual initial situation and the available resources. It is important to work out a few particularly suitable therapy modules and to motivate and empower the patient to take care of themselves in the long term through information or training.
Treatment of Polyneuropathies In the Department of Naturopathy At the Immanuel Hospital Berlin
About 5-10% of the inpatients treated with us show a diagnosis or co-diagnosis of polyneuropathy. As is increasingly noticeable for us in epidemic studies, the proportion of polyneuropathy of unclear etiology is increasing. Basically, the proportion of underlying causes such as type 2 diabetes mellitus as well as the condition after chemotherapy due to cancer increases among the specific causes.
The 5 classic naturopathic treatments offer activating, desensitizing, analgesic and stress-reducing elements for polyneuropathy.
As part of the inpatient therapy in the Department of Naturopathy at the Immanuel Hospital Berlin, a multimodal complex treatment is used, which provides for a treatment duration of 10-14 days, depending on the primary diagnosis and DRG [German Hospital Service].
The basis of the therapy is the 5 classic naturopathic treatments. In the field of nutritional therapy, nutritional medical aspects of the metabolic diseases associated with PNP, especially in the presence of a diabetic metabolic state or hepatopathy, are addressed. In nutritional counselling, the traditional Mediterranean diet, the whole food diet according to Leitzmann and basically plant-based diets are trained accordingly. If there are no contraindications, a 5-7 day therapeutic fasting according to Buchinger or a fasting-mimicking diet is initially prescribed. For some indications, pain-relieving and anti-inflammatory effects have been proven for fasting therapy by means of prolonged fasting. Although there are no specific studies for the diagnosis of polyneuropathy, the good effects of fasting have been regularly documented in the clinic’s experience.
Movement therapy takes into account the individual possibilities in terms of coordination, balance and muscle control. This means that highly personalized movement training takes place here under physiotherapeutic guidance. In addition to improving mobility, especially walking, strength training is also integrated, this against the background of the anti-inflammatory effect of myokines, which in turn are associated with muscle mass.
In the field of “Lifestyle Regulation Therapy” and mind-body medicine, methods for stress reduction and relaxation response are used according to individual preference. The focus is on meditation, autogenic training, progressive muscle relaxation according to Jacobson, but also Qigong, Tai Chi and Yoga. Yoga, on the other hand, strongly integrates elements of classic movement therapy.
In the field of phytotherapy, capsaicin is applied locally in low doses topically as a cream or in high doses as a patch. In addition to or supporting pain therapy, anxiolytic medicinal plants such as lavender, saffron or, if depression is present, St. John’s wort and turmeric are used. CBD and/or THC are used in individual cases for complementary symptomatic therapy.
In the field of physical therapy and hydrotherapy, exercise baths, water aerobics, water running as well as hydro-thermotherapy according to Kneipp with Kneipp showers, foot baths and wraps are used. In addition, foot vibration baths and foot massages are used for prevalent complaints in the area of the feet and the sole of the foot.
Systemic cryotherapy using a cold chamber is often used with good success. This leads to antinociceptive effects even in the short term, which have lasting effects for up to several months in the case of serial treatment over 5 therapies with -100 to -130 °C. Corresponding evidence is available for its use in rheumatoid arthritis as well as various musculoskeletal pain syndromes. The prerequisite for the use of the cryotherapy chamber is sufficiently safe mobility.
In addition, we use infusions with alpha-lipoic acid (ALA). For the administration of ALA in PNP, there is moderate evidence from meta-analysis; in everyday clinical practice, they repeatedly lead to significant acute improvements in symptoms. In addition, the blood levels of Vitamin B12 and Vitamin D are determined in all patients and, if necessary, medication is used.
Finally, acupuncture is treated according to appropriate proven acupuncture patterns. In addition, the needle mat is used, which can also be used for self-treatment afterwards.
Overall, such multimodal therapy can achieve at least a moderate improvement in the symptoms, especially the pain, but often also the sensory disorders in most patients.
 Fig. 4: Interdisciplinary patient discussion of the specialist staff in the context of multimodal therapy (MNS) at LMU. Source: D. lrnich [rerif]
Fig. 4: Interdisciplinary patient discussion of the specialist staff in the context of multimodal therapy (MNS) at LMU. Source: D. lrnich [rerif]
Treatment of Polyneuropathies At the Interdisciplinary Pain Outpatient and Day Clinic, LMU Munich, Campus Innenstadt
Patients with chronic pain with PNP are treated on an interdisciplinary basis, on an outpatient or day-care basis in the “Munich Naturopathic Pain Intensive Program” (MNS). The MNS is a multimodal day-care 4-week pain program in groups of a maximum of 8 patients, which has been established since 2001 and meets the quality criteria of “Interdisciplinary Multimodal Pain Therapy” (IMST, e.g. according to OPS procedure 8-91.x).
If PNP is chronic pain with corresponding restrictions on everyday activity as well as emotional and social stress, modern scientifically based pain medicine according to the biopsychosocial model (extended by socio-cultural and spiritual factors) assumes a chronic pain disorder that requires an intensive interdisciplinary treatment concept. The essential quality criteria of such concepts are the integrated interaction of different somatic, psychotherapeutic, movement therapeutic and physical-medical treatment approaches in a team that communicates well and regularly with each other [4]. The prerequisite for success is that the participating doctors, psychologists, therapists and nurses have a basic understanding of pain chronification (pain specialization) and pull together according to a jointly developed concept. Experience in the integration of selected naturopathic and complementary medical therapy methods, in the sense of integrative pain therapy into the treatment of PNP, supports desensitization and the internal conviction of control (self-efficacy) by learning self-applications as well as pain management through relaxation, creative and movement therapies (e.g. balance-promoting exercises of Qi-gong).
It is crucial to get to know and practice the wide range of different procedures within the framework of IMST in order to then implement the approaches that are personally perceived as helpful in everyday life. As a rule, patients are admitted to the group program for whom the usual conventional therapy methods have not provided sufficient relief, have not been tolerated or do not represent a permanent solution.
The procedures listed in Table 1 are used in the treatment of chronic pain in PNP. These are either offered in a small concept selected as part of outpatient treatment or fully implemented as a semi-inpatient group program over 4 weeks daily from 9:00 a.m. to 4:00 p.m. as part of the “Munich Naturopathic Intensive Program”.
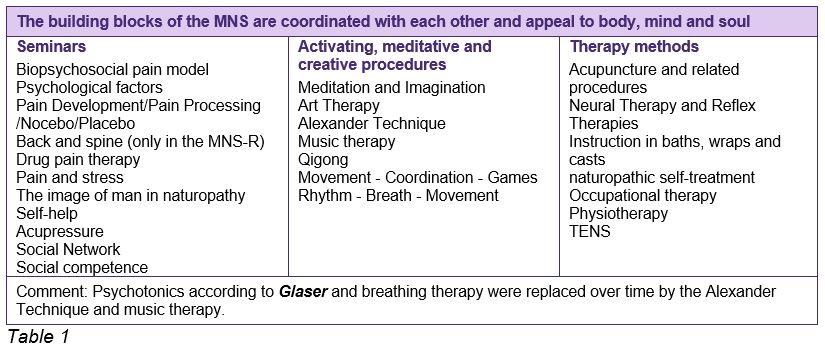
Seminars
Seminars are offered exclusively for the patients of the group program. In the outpatient setting, essential contents of the seminars are addressed individually for the patient in the context of medical and psychological care. The seminars, which last 60 or 75 minutes, are conducted by doctors, psychologists and nurses who specialize in integrative pain therapy. Emphasis is placed on the interactive character of the seminars.
Activating, Meditative And Practicing Procedures
A wide range of procedures are used to give patients the opportunity to assess the forms of application, techniques and effects of the respective procedure. The aim is to identify 1-2 procedures that are personally perceived as effective in order to integrate them into everyday life. The individual procedures are offered 4-8 times over the course of the 4 weeks in order to gain a deeper insight and to experience the value of deepening and repetition first-hand. This also includes the creative methods of art therapy and music therapy, which have now gained weight as part of multimodal pain therapy. The importance of unprocessed or stressful feelings for pain processing is well known.
Physical Medicine and Complementary Therapies Procedures
Various therapy methods (Table 1) are offered partly on an outpatient basis and entirely in a group setting. The goals are manifold:
- Immediate pain relief according to the stimulus-response principle of naturopathy with activation of endogenous antinociception (including descending pain inhibition, segmental inhibition)
- Desensitization of the increased level of arousal of nociceptive afferents
- Blood circulation promotion locally in the area of the affected limb
- Improvement of coordination and thus gait stability (also applies to Qigong and other movement therapies)
- sensory-perceptual training
- Elimination of postural insufficiency, incorrect postures and relieving postures
 Fig. 3: Mustard flour foot bath. Source: D. Irnich
Fig. 3: Mustard flour foot bath. Source: D. Irnich
According to experience the following procedures have proven to be particularly helpful in the treatment of polyneuropathy:
- Acupuncture electrostimulation locally, e.g. interdigital Bafeng (BaXie, Extra Point #10), anatomically nerve-related, e.g. GB34, St36, supplemented by manual acupuncture at distant points, system points according to TCM and microsystem acupuncture
- TENS: proximal to the affected region and/or paravertebral segmental (frequency 100 Hz or Han frequency, e.g. alternating between 2-5 Hz and 100 Hz every 3 seconds)
- Carbonic acid baths or, if a stronger stimulus is necessary, the mustard flour bath
- Physiotherapy with gait training and balance training
- Occupational therapy
- Qigong for strengthening coordination and stability
These methods have direct somatic effects, but as part of the multimodal therapy for chronic PNP pain, they require additional information on the modern biopsychosocial understanding of pain, the emphasis on knowledge of feelings as the most important factor in pain processing, and possibly the acceptance of limitations as part of the physiological aging process.
The aim of multimodal therapy is thus pain relief and functional improvement, the improvement of quality of life, the identification of pain-influencing emotional worlds, the motivation to cope with one’s own pain, the motivation for appropriate activity, the acceptance of biographical influencing factors, the recognition and modification of one’s own dysfunctional behavior and ultimately the improvement of the quality of life.
Conflict of interest: The authors state that there is no conflict of interest.

An Exclusive Translated Article for P2P Supporters
From the Monthly Publications of P2p
Published January 2026
From an article in zkm – Zeitschrift für Komplementärmedizin, Volume 17, Issue 6 2025
Translation & redaction by: Carolyn L. Winsor, P2P Consulting
© Copyright 2025, zkm, Dominik Irnich, Germany
AI Digital and online translation assistance utilized.
Literature
- Hanewinckel R, Drenthen J, van Men et al. Prevalence of polyneuropathy in the general middle-aged and elderly population. Neurology 2016; 87(18): 1892-1898
- Wiersma M, van der Star GM, Notermans NC et al. EXPRESS Study Consortium. Knowledge gaps in diagnosing chronic polyneuropathy: Review of national guidelines. J Peripheral Nerve Syst 2024; 29(4): 383-392. DOI: 10.1111/jns.12667
- Silsby M, Feldman EL, Dortch RD et al. Advances in diagnosis and management of distal sensory polyneuropathies. J Neurol Neurosurg Psychiatry 2023; 94(12): 1025-1039. DOI: 10.1136/jnnp-2021-328489
- Arnold B, Böger A, Brinkschmidt T, Casser HR et al. Implementation of interdisciplinary multimodal pain therapy according to OPS 8918: Recommendations of the ad hoc commission for interdisciplinary multimodal pain therapy of the German Pain Association. Schmerz 2018; 32(1): 5-14. DOI: 10.1007/s00482-018-0266-x.
** Translator notes: The highly respected KfN Clinic was first introduced to you in the article “Interim Results of the Ongoing Long-/Post-COVID Study” in January, 2023 (follow this link). And then in more depth in the article “Integrative Medicine” in September 2023 (follow this link).





