Causes Speak for the
Therapeutic Use of Antioxidants
Abstract
Hyperinflammation and oxidative stress play an important pathophysiological role not only in acute Covid-19 disease, but also in Long-Covid. In Covid-19 Vitamin C deficiency has been demonstrated and the benefit of supportive Vitamin C infusions has already been investigated. In Long-Covid excessive inflammation and reactive oxygen compounds are also co-triggers for fibrosis, thrombosis, immune dysregulation (autoimmune phenomena and viral persistence), fatigue, cognitive impairment and disturbances of the autonomic nervous system. The benefits of Vitamin C infusions – such as alleviation of fatigue, cognitive impairment and pain – have already been widely studied in other underlying diseases. Vitamin C is one of the most effective antioxidants, cofactor of relevant metabolic pathways and an important immunomodulator. The therapeutic use in Long-Covid is therefore very plausible and is confirmed by practical experience.
Keywords: Long-Covid, Post-Covid-19 Syndrome, Vitamin C, modulation, oxidative stress, antioxidants.
According to the (AWMF and NICE) definition under the term Long-Covid, symptoms are summarized which are in relation to Covid-19 and which persist or are newly added more than 4 weeks after the acute illness. Thus, this term also includes the Post-Covid syndrome. This includes symptoms that persist longer than 12 weeks (Figure 2).
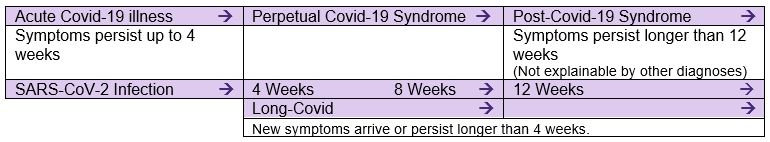 Figure 2: Covid-19 nomenclature based on AWMF Register No. 020/027 S1 Guideline Post-Covid/Long-Covid (Status 12.07.2021).
Figure 2: Covid-19 nomenclature based on AWMF Register No. 020/027 S1 Guideline Post-Covid/Long-Covid (Status 12.07.2021).
Long-Covid – Tired, Breathless and Unfocused
In the meantime Long-Covid has been investigated in numerous studies. A meta-analysis which took into consideration studies with more than 100 patients up to January 2021, has already identified 15 studies with a total of over 47,000 patients data(1). It reflects how diverse and whole-body affecting the symptoms can be, and at the same time shows that certain symptoms appear very frequently:
- Fatigue
- Headaches (inflammasome associated)
- Cognitive disturbances
- Breathlessness
Many affected people describe their condition as lacking in concentration, tired and breathless. The laboratory data from these studies referred causally to inflammation, vascular and cardiac disturbances(1). The causes for the frequently observed headaches are currently being intensively investigated. An important role seems to be played by the inflammasome: the part of our innate immune defence that is activated by pathogens or cellular stress and induces the release of inflammatory mediators.
The angiotensin-converting enzyme 2 (ACE2) is considered to be the entry point for SARS-
CoV-2 and – because it is expressed in almost all tissues – explains the diversity of symptoms (see Figure 3). Since ACE2 is also expressed on neurons, viral infection by SARS-CoV-2 could have direct negative effects on the autonomic nervous system. The most affected are the cardiovascular, gastrointestinal and genitourinary organ systems as well as thermoregulation(2).
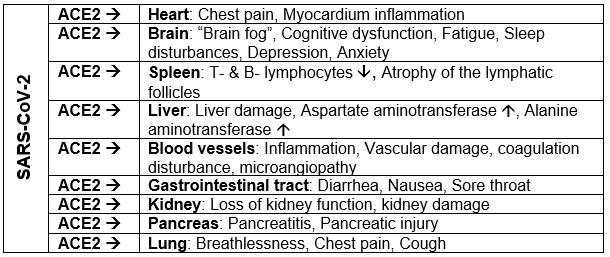 Figure 3: Multi-organ complications of Covid-19 and Long-Covid (based on(2)). The SARS-CoV-2 virus penetrates the cells of multiple organs through the ACE2 receptor and can cause a variety of damage that ultimately leads to numerous persistent symptoms.
Figure 3: Multi-organ complications of Covid-19 and Long-Covid (based on(2)). The SARS-CoV-2 virus penetrates the cells of multiple organs through the ACE2 receptor and can cause a variety of damage that ultimately leads to numerous persistent symptoms.
Inflammation and Oxidative Stress are Major Mechanisms in Long-Covid
According to WHO, Long-Covid is triggered by an interaction of different disease mechanisms of the acute disease. This view can also be found in the S1 Guideline of the AWMF on Post-Covid/ Long-Covid. As a result, especially 3 factors are decisively responsible for the pathophysiology:
- Hyperinflammation
- Vascular and nerve damage
- Immune dysregulation
- Autoimmunity
- Virus persistence, long-term infection
The authors of a state-of-the-art review from the British Medical Journal describe the mechanism and risk factors for Long-Covid. They see excessive inflammation and oxidative stress, i.e. an excess of reactive oxygen species (ROS) as important causes. Both are co-triggers for fibrosis, thrombosis, autoimmunity and disorders of the autonomic nervous system(2).
Inflammation and ROS Induced Fibroses in Lungs and Heart
In the alveoli of the lungs, chronic inflammation leads to the production of proinflammatory cytokines and ROS which are released into the surrounding tissues and the blood circulation. The resulting endothelial damage triggers the activation of fibroblasts which deposit collagen and fibronectin and thus lead to fibrotic changes in the lungs. Inflammation-related tissue hardening is also a serious problem in the heart. The fibrotic changes here are accompanied by an increase in cardiac fibromyoblasts and the chronic inflammation can lead to the death of the cardiomyocytes(2).
Inflammation and ROS Cause Brain Fog and Fatigue
In the brain the sustained immune response activates glial cells which can chronically damage neurons and are responsible for cognitive impairment. There is a disbalance of important neurotransmitters. The concentrations of kynurenine and quinolinic acid increase and through a strong glutamate influx leads to apoptosis of nerve cells. At the same time there is a deficiency of serotonin, dopamine and norepinephrine(3). B vitamins (B6, folic acid and B12) and Vitamin C are important for the new synthesis of these important messenger substances, which is why they are used therapeutically for Long-Covid. In addition, inflammation and disturbances of blood clotting increase the risk of thrombotic events and damage the blood-brain barrier, so that substances from the blood and leukocytes can penetrate the brain parenchyma(2). Chronic inflammation in the brain and at the neuromuscular nodes as well as circulatory disorders are also discussed as triggers for the frequently observed fatigue. Fatigue and rapid exhaustion can be further intensified by damage to skeletal muscles and fiber loss(2).
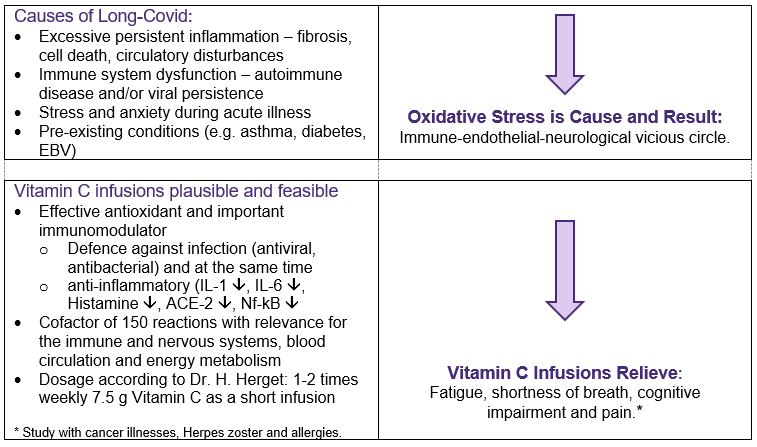 Figure 4: Oxidative stress is significantly involved in the development of Long-Covid symptoms. This makes the therapeutic use of antioxidants such as Vitamin C plausible (content in accordance with (5)).
Figure 4: Oxidative stress is significantly involved in the development of Long-Covid symptoms. This makes the therapeutic use of antioxidants such as Vitamin C plausible (content in accordance with (5)).
Immune Modulation is Crucial
After infection with SARS-CoV-2 concerted action by the immune system is necessary to control and/or to stop the replication. This rapid systemic immune reaction against SARS-CoV-2 includes the buildup of proinflammatory cytokines such as Interleukin-6 (IL-6) and tumor necrosis factor (TNF), the appearance of activated monocytes, followed by SARS-CoV-2 specific immunoglobulin M (IgM), IgA and IgG antibodies and of course interferon-ɣ producing T-cells. This corresponds to a curative inflammation with which the virus could no longer be isolated in the respiratory tract after 3 weeks.
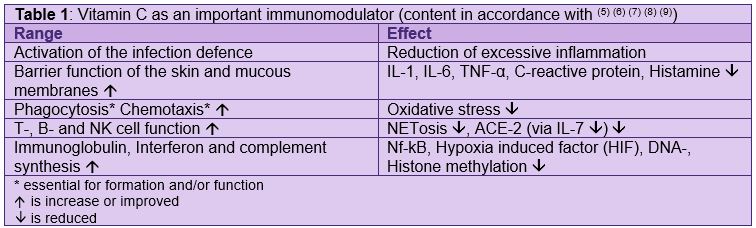
An excessive inflammation is counterproductive and harmful which – just like other viral infections – damages the immune system and organs of the lungs very much and thus increases the risk of pneumonia and sepsis. Therefore it is not sufficient to only treat against bacteria and viruses. Immune modulation is crucial(4). Immune modulation means to support the body’s own defences and at the same time protecting them from excessive inflammation. Phrased differently: to help the organism to respond appropriately to a pathogen without excessively damaging the host. Vitamin C plays an important role here: On the one hand it is important for many components of the infection defence (barrier function, formation of immunoglobulin and interferon, lymphocyte function, etc.) and at the same time curbs the damages of hyperinflammation (IL-1, IL-6, TNF-α, histamine lowering, antioxidant, etc.; see Table 1 next page; see Figure 4 previous page).
The immune dysregulation thought to be the cause of Long-Covid interestingly goes in both directions: hyperactivity with autoimmune phenomena and a weakened defence against infections with viral persistence and a kind of long-term infection. A recently published longitudinal analysis study with 309 Covid-19 patients examined blood and nasal swabs with a variety of molecular biochemical methods. As a result 3 factors were found that greatly increased the risk of Long-Covid(10):
- High viral load at the onset of the illness
- Autoantibodies
- Pre-existing illnesses (EBV infection in the anamnesis, Type 2 diabetes)
The reactivation of any possible pre-existing inactivated Epstein-Barr virions (EBV) is also seen in practice in the development of Long-Covid.
Also interesting in this study is the observation that subclinical autoantibodies correlate negatively with SARS-CoV-2 antibodies, that is the more autoantibodies the fewer antibodies against SARS-CoV-2(10).
A weak immune response at the beginning of acute Covid-19 illness is also seen as an important predictor of Long-Covid in a recent multicenter cohort study from Switzerland(11). The risk of permanent symptoms was greatly increased in patients with low IgG3 and IgM levels at the beginning of the acute illness. Bronchial asthma in the anamnesis also seems to be a risk factor which is plausibly explained by the authors. The secretion of IgM and especially of IgG3 by B cells is induced by interferon and antagonized by IL-4 which is increasing produced in asthma. This may also explain why asthma increases the risk of Long-Covid(11). A Vitamin C deficiency which accompanies many chronic inflammatory diseases such as asthma, arthritis, diabetes, etc., also most likely plays a role here – as mentioned Vitamin C is important for formation of interferon (See Table 1). A deficiency should be avoided or treated particularly quickly especially in times with an increased risk of infection. Low IgG3 levels are also associated with chronic fatigue syndrome, and as everybody knows fatigue is the main symptom of Long-Covid.
Severity of the Acute Illness Affects Long-Covid
According to the previously mentioned Swiss study Long-Covid symptoms emerge with severe Covid-19 cases approximately 2 to 6.5 times more frequently than with mild ones. Only odor and taste disorders establish an exception(11).
Especially interesting is the connection between the severity of the acute illness and mental suffering with Covid-19 patients who did not have to go into the hospital. This is shown in the data from 7 prospective cohort studies from 6 northern European countries (Denmark, Iceland, Estonia, Norway, Sweden and Great Britain). Patients who were not at all forced into bed by the infection more rarely developed depression and anxiety symptoms in comparison with the healthy controls – possibly because afterwards they could return sooner to a little more normal life. Conversely, among Covid patients who were bedridden for at least 7 days, there was a significantly increased proportion with signs of depression (+61%), anxiety (+43%) and sleep disorders (+41%) that persisted over the observation period of up to 16 months. In particular the authors see 2 factors that could explain the long-term psychological consequences after a severe course of Covid-19: the fears associated with the illness and the inflammatory process during the acute phase(12). These results send a reminder for an increased watchfulness concerning the mental health of patients who are going through a severe Covid-19 illness in isolation at home.
The connection with Vitamin C is obviously also here. Studies with supportive Vitamin C infusions for Covid-19 show not only an improvement in oxygen supply and a reduction of inflammation, but also less severe courses(5) (13). The connection between traumatic experiences and oxidative stress is also interesting because post-traumatic stress disorder induces oxidative stress in the hippocampus and thus causes memory loss. This could be mitigated through experimental studies for Vitamin C(14). Oxidative stress also causes neuronal damage in other brain areas responsible for regulating stress, emotions, anxiety and memory processing – for example, in the amygdala and frontal cortex.
Keeping An Eye on Vitamin C Deficiency
Infections such as SARS-CoV-2 induce oxidative stress and high consumption of Vitamin C. They often lead to a Vitamin C deficiency(13).
In Long-Covid the Vitamin C status has not yet been studied, but a deficiency is likely due to heavy consumption during the acute illness and should be clarified during treatment. Not the least because the symptoms of Vitamin C deficiency are very similar to those of Long-Covid: fatigue, poor performance, depressive mood, impairment of mental well-being, pain, susceptibility to infections and slowed recovery after illness.
Vitamin C Infusions for Fatigue, Cognitive Disturbances and Pain are Plausible and Feasible
Fatigue often emerges with cancer, after infections and in autoimmune diseases – all diseases that are accompanied by a high magnitude with oxidative stress. Oxidative stress is an obvious contributory cause of fatigue and thus a promising biomarker for treatment (see Figure 4).
In a systematic review, the feasibility of high-dose intravenous Vitamin C in fatigue was evaluated and 9 clinical studies with 720 patients suffering from fatigue/exhaustion were identified(15). In the predominant number of studies the contributory cause of fatigue was from an oncological disease. One study also examined in each case the effects on patients with herpes zoster, allergies, condition after surgery and supposedly healthy full-time employees. Of the 4 controlled studies, 3 observed a significant decrease in fatigue in the Vitamin C group compared to the control group (p <0.005). In the observational as well as the before-after studies a reduction of fatigue was also established, whereby in the 4 studies with statistical comparison of the pre-post values the therapeutic effect was significant. Accompanying symptoms of exhaustion such as sleep disturbances, cognitive disorders, depression and pain were also frequently alleviated in patients receiving intravenous Vitamin C.
Vitamin C infusions can quickly and efficiently remedy deficiency conditions. Vitamin C is thus again available as a cofactor for important functions (e.g. neurotransmitter synthesis) and as an important antioxidant. In the observational study in herpes zoster a Vitamin C dose of 7.5 g was used 2 to 3 times a week. In addition to pain reduction a significant improvement in fatigue and cognitive dysfunction was observed. The same dose has been used in the treatment of allergies where fatigue is also a symptom impairing the quality of life.
Case Report from Harald Herget, MD
Patient, 16 years old, vaccinated 2 times, approx. 10 days after the 2nd vaccination came with a positive PCR test and typical symptoms of Covid infection with fever, cough, mild shortness of breath, cervical lymph node swelling and a pronounced fatigue syndrome with physical and mental exhaustion. Treatment by the family doctor occurred symptomatically. After approx. 12 days significant improvement of the complaint picture. Fatigue, exhaustion and lack of concentration persisted. The following PCR test was negative. After approx.. 4 weeks of renewed deterioration with cough, shortness of breath, pressure in the heart region with increased extrasystoles and tachycardia. The fatigue symptoms also worsened significantly. PCR test was negative. After 6 weeks 1st Vitamin C infusion (Pascorbin 7.5 g). In addition: Vitamin B1-Injectopas 100 mg, Vitamin B6-Injectopas 25 mg, Vitamin B12-Injectopas 1000 µg, Folic Acid Injectopas 5 mg, Lymphdioral Injectopas L, Infection1-Injectopas, Broncho-Injectopas and Cor Plus Injectopas, 1 ampule each. Already after the 2nd treatment a significant improvement could be documented. This treatment was carried out 1 x weekly for 5 weeks until complete freedom from complaints.
Conflict of Interest
Claudia Vollbracht works as a consultant in medical science at Pascoe Pharm Präparate GmbH.
Harald Herget has been a consultant for Pascoe Pharm Päparate GmbH for 40 years.

An Exclusive Translated Article for P2P Supporters
From the Monthly Publications of P2P
Published February 2023
Translated and re-published in an effort to spread the information and research to as many practitioners of complementary, integrative and energy medicine as possible:
From an article in Erfahrungsheilkunde, Volume 71, Issue #5, 2022
Machine Translation by Lernout & Hauspie, LogoMedia & Promt
Translation & redaction by: Carolyn L. Winsor, P2P Consulting
© Copyright 2022, EHK 2022:71: 252-257 | 2022. Thieme. All rights reserved.
Bibliography
EHK 2022:71: 252-257
DOI 10.1055/a-1718-7472
ISSN 0014-0082 2022. Thieme. All rights reserved.
Karl F. Haug Verlag in MVS Medizinverlage Stuttgart GmbH & Co.
KG, Oswald-Hesse-Straße 50,70469 Stuttgart Germany
Literature
- Lopez-Leon 5, Wegman-Ostrosky T, Perelman C et al. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci Rep 2021; 11(1): 16144
- Crook H, Raza S. Nowell J et al. Long covid-mechanisms, risk factors, and management. BMJ 2021; 374: n1648
- Boldrini M, Canoll PD, Klein RS. How COVID-19 affects the brain. JAMA Psy 2021; 78(6): 682-683
- Vollbracht C, Guendling PW. Immunmodulation mit Vitamin C. EHK 2017; 66:36-43
- Vollbracht Kraft K. Oxidative stress and hyper-inflammation as major drivers of severe COVID-19 and long COVID: Implications for the benefit of high-dose intravenous vitamin C. Front Pharmacol 2022; 13: 899198
- Carr AC, Maggini S. Vitamin C and immune function. Nutrients 2017; 9(11): 1211
- Ang A, Pullar JM, Currie MJ et al. Vitamin C and immune cell function in inflammation and cancer. Biochem Soc Trans 2018; 46(5): 1147-1159
- Lee Chong T, Ahearn EL, Cimmino L. Reprogramming the epigenome with vitamin C. Front Cell Dev Biol 2019; 7: 128
- Mousavi S. Bereswill S. Heimesaat MM. Immunomodulatory and antimicrobial effects of vitamin C. Eur J Microbiol Immunol (Bp) 2019; 9(3): 73-79
- Su Y, Yuan D, Chen DG et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell Physiol Biochem 2022; 185(5): 881-895.e20
- Cervia C, Zurbuchen Y, Taeschler Petal. Immunoglobulin signature predicts risk of post-acute COVID-19 syndrome. Nat Commun 2022; 13(1): 446
- Magnusdottir I, Lovik A, Unnarsdottir AB et al. Acute COVID-19 severity and mental health morbidity trajectories in patient populations of six nations: An observational study. Lancet Public Health 2022; 7(5): e406-e416
- Holford P, Carr AC, Zawari Metal. Vitamin C intervention for critical COVID-19: A pragmatic review of the current level of evidence. Life 2021; 11: 1166
- Alzoubi KH, Shatnawi AF, Al-Qudah MA et al. Vitamin C attenuates memory loss induced by post-traumatic stress like behavior in a rat model. Behav Brain Res 2020; 379: 112350
- Vollbracht C, Kraft K. Feasibility of vitamin C in the treatment of post viral fatigue with focus on long COVID, based on a systematic review of IV vitamin C on fatigue. Nutrients 2021; 13(4): 1154




